Diabetes Ireland is delighted to launch its Pre-Budget Submission 2024.
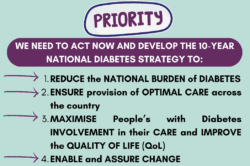
In 2024, we are urging the Minister for Health, the Department of Health, and the Government to prioritise two very important initiatives which are:
To set up a task force to develop a 10-year National Diabetes Strategy (Cost: negligible)
To improve access to any form of continuous glucose monitoring (CGM) (Cost: €5 million)
CLICK HERE TO READ THE PRE-BUDGET SUBMISSION 2024
How can you help? Take Action Today and Have Your Voice Heard!
We are asking every member of the diabetes community to support this Pre-Budget Submission by contacting local TDs by sending them the following letter with Parliamentary Questions for the Minister for Health, Stephen Donnelly TD.
Please download the letter, adapt it accordingly to your needs, and send it to the TDs in your constituency. See the list of TDs from your constituency HERE. For any queries, contact [email protected].
Click and see the Letter Template to send to your TD
WHY?
Diabetes is a serious global public health issue which has been described as the most challenging health problem in the 21st century with high individual, social and economic burden (1,2). A s a leading cause of morbidity and mortality, affecting an estimated 308,000 people in Ireland (2-5), and the most prevalent chronic condition in people between 45 to 74 years of age with a prevalence rate just slightly behind cardiovascular disease in people over 75 years (6,7), diabetes places a significant burden on society and presents a growing challenge for the national economy (8-10).
Despite the Sláintecare reform which provided investment in improving diabetes care in primary care settings (11-12), and the positive work of the HSE National Diabetes Clinical Programmes, which have produced very detailed models of care for both Type 1 and Type 2 Diabetes (13-16), the lack of available resources to implement the recommendations of these documents mean people living with diabetes are suffering from a postcode lottery service when it comes to diabetes services. Diabetes Ireland survey on “Accessing Diabetes Services in Ireland” conducted earlier this year shows more than a third of respondents already have diabetes-related complications or comorbidities, and almost half of people with type 2 diabetes pay privately for their care.
Almost all children had at least two diabetes appointments in 2022, and 67% of them had three or more appointments. Among adults, 13% have not had any appointment in 2022. Almost one-third of those who had had only one appointment. Moreover, not everyone had received their annual check-ups (haemoglobin A1C, cholesterol levels, eye check, etc.). This does not fully meet the clinical guideline recommendations of two diabetes appointments per annum for adults living with diabetes and essential annual reviews (17).
SEE DETAILED SUMMARY SURVEY FINDINGS
-
ASK 1: – TASKFORCE TO DEVELOP A 10-YEAR NATIONAL DIABETES STRATEGY
The economic burden of diabetes on the Irish healthcare system is now a major challenge for the government and the Health Service Executive (HSE). The high cost of diabetes is mainly caused by the treatment of complications (surgeries, hospitalisations), many of which could be avoided with earlier detection, greater awareness of symptoms, better access to newer treatments and diabetes technologies, multidisciplinary teams including significant gaps in current services that need to be tackled in order to provide optimum diabetes care to everyone in need. With no data – diabetes registry nor clinical audits, we cannot even fully identify what the gaps and issues are. From what we know, despite the best efforts of current diabetes staff, the delivery of diabetes services in Ireland is at best piecemeal, uncoordinated and unstructured (17-19).
Therefore, to improve diabetes care, we need to collectively act now and decide what future care for people with diabetes will look like. Diabetes Ireland is calling for the setting up of a diabetes task force of relevant stakeholders (healthcare professionals, academics and researchers, patient advocates, Department of Health and HSE representatives) to develop a 10-year National Diabetes Strategy that provides vision, leadership, goals, and priorities, as well as identifying and securing the future funding required to provide optimum care for every person living with diabetes in Ireland. A similar initiative – setting up a National Cancer Strategy a few years back (20, 21) hugely improved access to and quality of care for those affected by cancer. We need similar steps to support people with diabetes and their families, friends, carers, employers, researchers, doctors, nurses and all other health professionals involved in diabetes care.
-
ASK 2: – €5 MILLION FOR WIDENING ACCESS TO CGM
For those living with diabetes, in particular with Type 1 diabetes, frequent daily glucose monitoring is essential to maintain safety and well-being, and reduce the risk of short and long-term diabetes complications. it is recommended that people using insulin check their glucose levels a minimum of 4 times per day, but in reality, they need to check a lot more often – before any meal, if they feel unwell, before bed, at nighttime etc. This level of frequent testing using traditional finger-pricking devices can be painful, inconvenient and difficult to achieve as people go about their daily lives, and it provides one-off information about current glucose levels only (22-25).
For the last couple of years, Continuous Glucose Monitoring (CGM) changed the way people manage diabetes – this revolutionary technology helps people living with type 1 diabetes and all others using intensive insulin therapy move away from the hassle of multiple daily finger pricks (to check their blood sugar levels) and instead enables needle-free monitoring of blood glucose via a sensor inserted on the arm. it also provides contextual information – trends (shows whether the glucose levels are rising or falling or are stable) and some provide alarms when the glucose levels drop or rise. This information enables better decision-making about insulin dosing and many other activities (22-27). CGM is also used as part of an automated insulin delivery system – an artificial pancreas system (28).
Many international societies and guidelines recommend CGM use as an essential part of Type 1 diabetes management (22-25). Updated NICE (2022) guidelines used across the UK recommend that CGM/FSL (FreeStyle Libre intermittently scanned sensor (26-27), which is also a type of CGM) should be provided to all people with diabetes using insulin (29-31). In Ireland, NICE guidelines are used for adults with Type 1 diabetes, but the last edition was launched in 2018 (16) and has not included this emerging technology by then. The same year, in line with the recommendations of the Health Technology Assessment Group (HTAG), the FSL device (a form of Flash Glucose monitoring that requires users to scan the sensor on their arm) was made available on an individualised basis to children and young adults with type 1 diabetes (age 4-21 years) through the Primary Care Reimbursement Scheme (PCRS). This has resulted in inequity of access and discrimination with devices provided based on age rather than clinical need (32). See more about this inequity in Diabetes Ireland ‘Accessing FSL survey’ conducted in 2021.
Differences in routes of access to technologies approved for funding exist according to system type and components. For example. Dexcom CGM is available with no age restriction, and the most recent model (G7) is available on prescription only. A HIQA Rapid Health Technology Assessment of CGM in Adults with Type 1 diabetes has been requested by the Minister for Health Stephen Donnelly at the end of 2022 and has been recently completed (2023) – we are awaiting official recommendations now. In line with international best proactive, the National Clinical Programmes (NCP) for Diabetes is requesting a broadening of the criteria for the provision of a form of CGM to all individuals living with Type 1 diabetes in Ireland.
Bearing in mind that many people with Type 1 diabetes already use CGM in Ireland, securing €5 million by the Government in the Budget 2024, will facilitate more equitable access and reduce disparities for those living with Type 1 diabetes management, outcomes and quality of life. Diabetes Ireland fully supports this request and with the main request to set up the Taskforce to develop the National Diabetes Strategy, we hope that people with diabetes will be provided the best available treatment, including diabetes technology, based on their clinical need.
References:
-
World Health Organization. The top 10 causes of death 2019 [Available from: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death]
-
Diabetes Ireland. Pre-Budget Submission 2023. [Available from: https://www.diabetes.ie/wp-content/uploads/2022/09/Pre-Budget-Submission-2023-Diabetes-Ireland.-OK.pdf]
-
Parliamentary Question 46154/21 September 28th answer in writing October 15th 2021 [Available from https://www.oireachtas.ie/en/debates/question/2021-09-28/661/?highlight%5B0%5D=46154&highlight%5B1%5D=21]
-
The Scottish Diabetes Survey 2021. Scottish Diabetes Group. [Available from: https://www.diabetesinscotland.org.uk/wp-content/uploads/2023/02/Diabetes-Scottish-Diabetes-Survey-2021-final-version.pdf]
-
Central Statistics Office. Census of Irish Population 2022. Preliminary findings [Available from: https://www.cso.ie/en/releasesandpublications/ep/p-cpr/censusofpopulation2022-preliminaryresults/]
-
Evidence for Policies to Prevent Chronic Conditions (EPICC) Team. Prevalence Estimates of Chronic Conditions in Ireland [policy brief]. 2022. [Available from: https://www.lenus.ie/handle/10147/632829]
-
Evidence for Policies to Prevent Chronic Conditions (EPICC) Team. Chronic Disease Burden in Ireland. Report. 2022 [Available from: https://www.lenus.ie/handle/10147/632830].
-
O’Neill KN, McHugh SM, et al. Health service utilization and related costs attributable to diabetes. Diabetic Medicine. 2018;35(12):1727-34.
-
Nolan J., O’Halloran D, McKenna TJ, et al. The Cost of Treating Type 2 Diabetes (CODEIRE). Irish Medical Journal. 2006;99(10):307-10.
-
Central Statistics Office. Health Expenditure in Ireland 2022. [Available from: https://www.cso.ie/en/releasesandpublications/ep/p-sha/systemofhealthaccounts2021/provisionalhealthexpenditureestimatesfor2022/]
-
Government of Ireland. Slaintecare. Right Care. Right Place. Right Time. Sláintecare Implementation Strategy & Action Plan 2021 — 2023. 2021
-
Integrated Care Programme for the Prevention and Management of Chronic Disease. National Framework for the Integrated Prevention and Management of Chronic Disease in Ireland 2020-2025. Health Service Executive, ; 2020.
-
National Clinical Programme for Diabetes Working Group. Model of Integrated Care for Patients with Type 2 Diabetes – A Guide for Health Care Professionals. 2018.
-
National Office of Clinical Audit, . National Paediatric Diabetes Audit Feasibility Study. Dublin: National Office of Clinical Audit; 2022.
-
National Clinical Programmes for Diabetes and Paediatrics. Model of Care for All Children and Young People with Type 1 Diabetes. 2015
-
Department of Health (2018) Adult type 1 diabetes mellitus (NCEC National Clinical Guideline No. 17). Available at: http://health.gov.ie/national-patient-safety-office/ncec.
-
Diabetes Ireland. Accessing and using diabetes health services: the ‘Patient Experience’ survey of people living with diabetes in Ireland. 2023. [Available from: https://www.diabetes.ie/accessing-diabetes-services-in-ireland-2023/]
-
Diabetes Ireland. Pre-Budget Submission 2022. [Available from: https://www.diabetes.ie/wp-content/uploads/2021/07/Diabetes-Ireland-Pre-Budget-Submisison-2022.pdf]
-
O’Donnell M, Niamh Smyth, Sean Dinneen, on behalf of the National Clinical Programme for Diabetes. National Survey of Diabetes Care Delivery in Acute Hospitals.; 2018.
-
Department of Health. National Cancer Strategy 2017-2026. [Available from: https://www.gov.ie/en/publication/a89819-national-cancer-strategy-2017-2026/]
-
National Cancer Strategy 2017-2026. [Available from: https://assets.gov.ie/9315/6f1592a09583421baa87de3a7e9cb619.pdf]
-
Tauschman M., Forlenza G., Hood K. et al. ISPAD Clinical Practice Consensus Guidelines 2022: Diabetes Technologies: Glucose Monitoring. Pediatr Diabetes. 2022;23:1390–1405
-
De Bock M., Codner E., Craig M. et al. Clinical Practice Consensus Guidelines 2022: Glycemic targets and glucose monitoring for children, adolescents and young people with diabetes. Pediatr Diabetes. 2022;23:1270–1276.
-
Holt RIG, DeVries JH, Hess-Fischl A., et al. The management of type 1 diabetes in adults. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia. 2021;64(12):2609-52.
-
American Diabetes Association Professional Practice C, Draznin B, Aroda VR, Bakris G, Benson G, Brown FM, et al. 7. Diabetes Technology: Standards of Medical Care in Diabetes-2022. Diabetes Care. 2022;45(Suppl 1):S97-S112.
-
Prigge R, McKnight JA, Wild SH, Haynes A, Jones TW, Davis EA, et al. International comparison of glycaemic control in people with type 1 diabetes: an update and extension. Diabetic medicine : a journal of the British Diabetic Association. 2022;39(5):e14766.
-
Tyndall V, Stimson RH, Zammitt NN, Ritchie SA, McKnight JA, Dover AR, et al. Marked improvement in HbA1c following commencement of flash glucose monitoring in people with type 1 diabetes. Diabetologia. 2019;62(8):1349-56.
-
Sherr JL, Heinemann L, Fleming GA, Bergenstal RM, Bruttomesso D, Hanaire H, et al. Automated insulin delivery: benefits, challenges, and recommendations. A Consensus Report of the Joint Diabetes Technology Working Group of the European Association for the Study of Diabetes and the American Diabetes Association. Diabetologia. 2023;66(1):3-22.
-
National Institute for Health and Care Excellence (NICE). NG17 Type 1 diabetes in adults: diagnosis and management [B] Evidence reviews for continuous glucose monitoring in adults with type 1 diabetes. 2022.
-
National Institute for Health and Care Excellence (NICE). NG18 Type 1 diabetes in children and young people: diagnosis and management [B] Evidence reviews for continuous glucose monitoring in children and young people with type 1 diabetes. 2022.
-
National Institute for Health and Care Excellence (NICE). NG28 Type 2 diabetes in adults: diagnosis and management [C] Evidence reviews for continuous glucose monitoring in adults with type 2 diabetes. 2022.
-
Diabetes Ireland. Accessing and Using Flash Glucose Monitoring (Freestyle Libre) in Ireland 2021 Survey Report. Dublin, Ireland: 2022