Diabetes Ireland has launched its 2022 Pre-budget submission and is proposing 8 immediate actions for implementation which will improve the quality of life for over 225,000 people living with diabetes and reduce the long term costs of preventable diabetes complications. The submission is focused on a range of deliverable actions that are person-centred, cost effective and builds on existing HSE commitments to tackle chronic conditions including diabetes.
One of these Actions is Psychology Services for People with Diabetes
Psychology Services
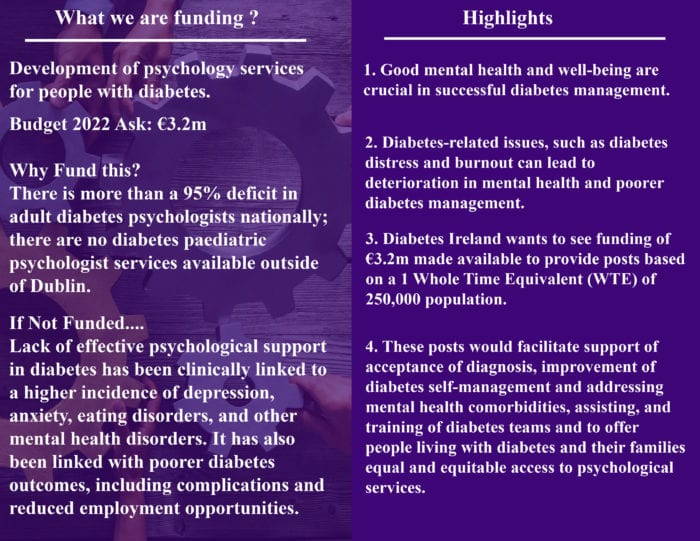
Development of psychology services for people with diabetes
Good mental health and well-being are the core of all aspects of life and are crucial in successful diabetes management. People living with diabetes face the burden associated with the condition every hour of every day. It requires continuous self-management and the necessity to make multiple medical decisions daily. This burden is reflected in the significantly higher incidence of depression, anxiety, and other mental health disorders, including eating disorders in the diabetes population when compared to other populations.
Some specific diabetes-related issues, such as diabetes distress and burnout, lead not only to significant deterioration in mental health but also to poorer diabetes management and outcomes. This in turn can lead to reduced motivation and capacity to deal with the responsibilities associated with diabetes which can result in a higher incidence of depression and the development of expensive diabetes-related complications and a reduced quality of life.
In the current social and economic circumstances within Ireland, the physical and mental health of people with diabetes of all ages is not at the top of any agenda. Although recognised by the HSE, psychosocial support in diabetes care is not formally embedded as part of diabetes management and not in line with diabetes-related health-services delivery in Ireland.
Presently, there is a 95% deficit of diabetes psychologists in adult diabetes services in acute hospitals and there is no access to dedicated diabetes psychology services in primary care. For children with diabetes, there is limited access to 3 paediatric psychologists within national HSE paediatric diabetes services, however, they are all based in Dublin with no access elsewhere in the country.
With so little resources available, the gap in access to psychological support for people living with diabetes in Ireland is significant whereas the need to assess and deal with the psychological burden is substantial. To address this huge gap, Diabetes Ireland wants to see funding of €3.2m made available to provide the following posts based on a 3 Whole Time Equivalent (WTE) per 250,000 population:
- 18 WTE clinical psychologists for Acute Diabetes Services nationally. This will give each acute hospital diabetes multi-disciplinary team (MDT) 1 WTE post.
- 6 WTE diabetes psychology resource allocated to each Community Diabetes Specialist Team Hub (32) under the Integrated Model of Care for the Prevention and Management of Chronic Disease Implementation Guide.
- 5 WTE clinical psychologist for each diabetes paediatric service nationally (14).
These posts will play a critical role in:
- Supporting adjustment to an acceptance of the diabetes diagnosis.
- Improving diabetes self-management through supporting behaviour change and adherence to diabetes care regimens and therefore reducing the prevalence of diabetes-related complications and mortality.
- Addressing mental health comorbidities (e.g. depression, anxiety, diabetes distress, eating disorders) through individual and group psychotherapeutic intervention, as people living with diabetes are at much higher risk of serious mental health disorders.
- Providing complex psychological formulation and neuropsychological assessment.
- Assisting and training the diabetes MDT in psychological aspects of diabetes, recognition of psychological challenges and basic support provision.
- Offer people living with diabetes and their families equal and equitable access to psychological services based on need, not ability to pay or geographical location, as in line with Sláintecare priorities.
Diabetes Ireland contacted all TDs and Senators on Wednesday 14 July on behalf of our community asking them to make representations on this and the other issues contained in our Pre-budget submission. Some of our active volunteers’ groups also followed up locally with their own local representatives. We are now asking you to Act. We need your help to highlight this issue once again in advance of the upcoming budget.
Call for Action: What Can I do?
-
- Copy the template below into an email and if you wish add your personal story and reasons why this problem matters to you.
- Find your local TD’s (constituency) https://www.oireachtas.ie/
- Send your email to your local politicians.
Email/Letter Template
Dear (INSERT NAME OF TD)
I am a constituent and regular voter in your area. I/my family member have/has lived with [INSERT THE TYPE OF DIABETES] diabetes for [INSERT YOUR DIABETES DURATION] years. As you will know, good mental health and well-being are the core of all aspects of life and are crucial in successful diabetes management. People living with diabetes face the burden associated with the condition every hour of every day. It requires continuous self-management and the necessity to make multiple medical decisions daily. Sometimes this can be a struggle (write here your personal story and the reason why you would like to highlight this particular issue to politicians).
In the current social and economic circumstances within Ireland, the physical and mental health of people with diabetes of all ages is not at the top of any agenda. Although recognised by the HSE, psychosocial support in diabetes care is not formally embedded as part of diabetes management and not in line with diabetes-related health-services delivery in Ireland.
Presently, there is a 95% deficit of diabetes psychologists in adult diabetes services in acute hospitals and there is no access to dedicated diabetes psychology services in primary care. For children with diabetes, there is limited access to 3 paediatric psychologists within national HSE paediatric diabetes services, however, they are all based in Dublin with no access elsewhere in the country.
With so little resources available, the gap in access to psychological support for people living with diabetes in Ireland is significant whereas the need to assess and deal with the psychological burden is substantial. To address this huge gap, people with diabetes wants to see investment in the diabetes specific psychology services. Therefore, I am writing to you to ask for your support by asking the Minister for Health if he will provide funding to develop psychological services for people living with diabetes in Ireland.
Parliamentary Questions to ask the Minister for Health
- To ask the Minister for Health will he provide funding to appoint a Clinical Psychologist to each acute hospital diabetes multi-disciplinary team; does he accept that psychosocial support in diabetes care is not formally embedded as part of diabetes management and if he will make a statement on the matter.
- To ask the Minister for Health will he provide a diabetes psychology resource to each Community Diabetes Specialist Team Hub under the Integrated Model of Care for the Prevention and Management of Chronic Disease Implementation Guide; does he accept that access to psychosocial support in these teams should be made available and if he will make a statement on the matter.
- To ask the Minister for Health will he provide funding to appoint a 0.5 WTE Clinical Psychologist to each acute hospital diabetes paediatric diabetes team; does he accept that psychosocial support in paediatric diabetes care should be available in each team; why is there no access to this support outside of Dublin paediatric diabetes services; will he make a statement on the matter.
- To ask the Minister for Health will he provide funding to appoint a Clinical Psychologist to my diabetes multi-disciplinary team in [INSERT YOUR HOSPITAL OR COMMUNITY HEALTH CENTRE] anytime soon.
Further information on this issue can be found at https://www.diabetes.ie/advocacy-call-to-action/psychology-services/
Thank you for your time in considering my request.
I hope to hear from you in due course.
Yours sincerely,
Your Name, Address, Email
To read the full Pre Budget Submission, click here.
Please note there are many other important issues we plan to highlight and advocate for going forward. implementation and we will be working with all stakeholders to do this in a strategic way.
Our advocacy work is important in giving our diabetes community a voice to be heard, become a member today, click here.
To read Easier Access to Mortgage Protection Cover, click here.
Call to action July 2021